Nigeria’s primary healthcare system faces many different challenges, and Benue State serves as a stark example of these struggles. Here, the dream of accessible, quality healthcare remains out of reach of rural areas, as communities are forced to resort to dilapidated and ill-staffed public healthcare facilities to survive.
A small bunch of Catholic faithful gathered at the compound that housed the Mbadam Primary Health Care Centre in Gboko, Benue State. If one didn’t know any better, one would assume that the crowd here offered prayers to the sick since the health centre didn’t seem to provide any help.
A man in front of the crowd filed out carrying a huge wax figure of the Virgin Mary, with the rest of the crowd trailing behind. Since it was bereft of equipment to cater for the sick and the injured, community members rarely visited the facility, Aondona Iorseer told me. Nowadays, villagers often travel to Gboko’s main town if they require any medical assistance.
“The workers here try, especially for pregnant women who come for anti-natal and things like malaria, but for anything serious, we have to go to Gboko,” he said through an interpreter, fingering the rosary in his hand.
A staff member, who later identified himself as Joseph, showed up, and feelers from him, was that the staff were performing miracles with what they had at the facility.
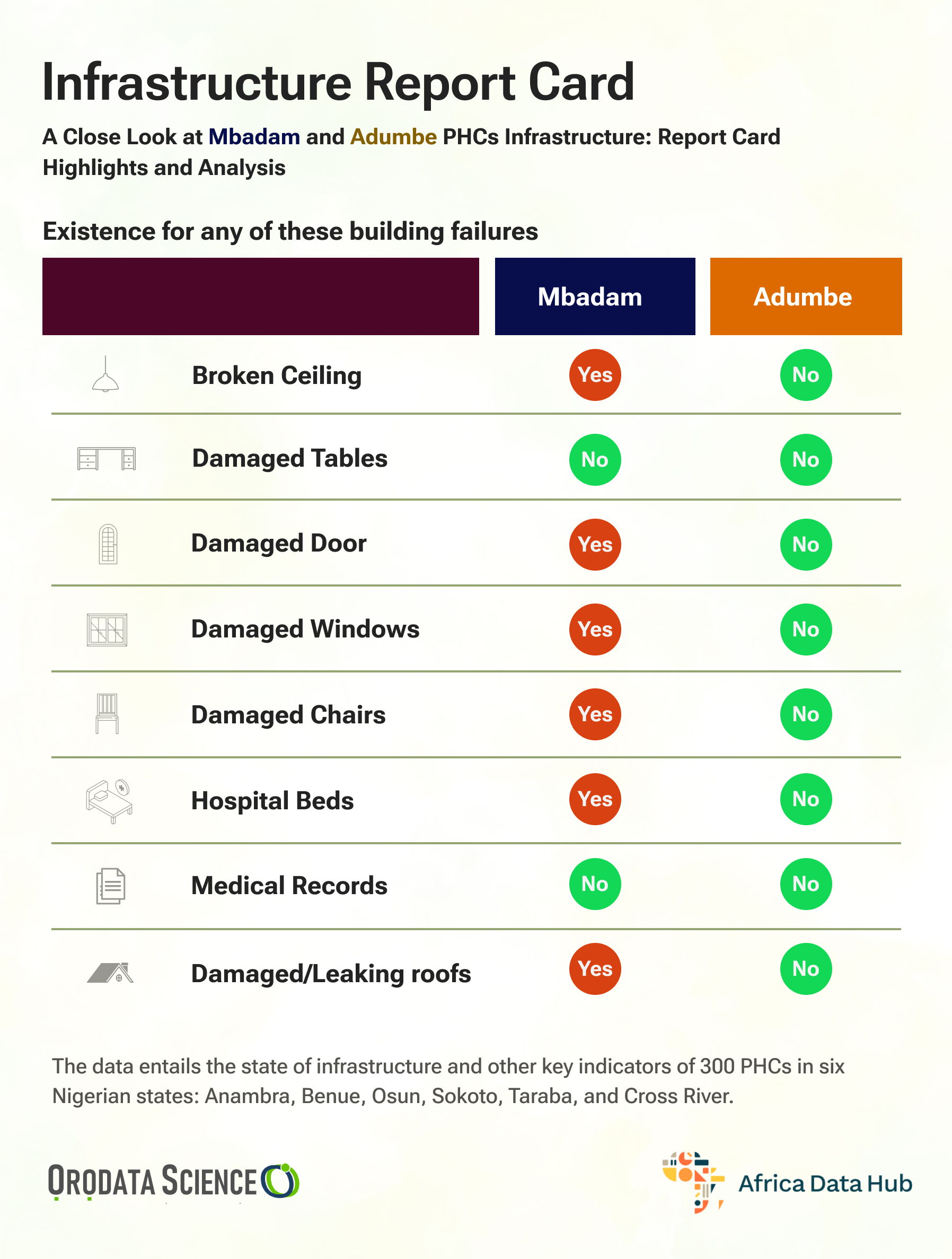
What is referred to as the Mbadam Health Centre is a small bungalow of about 5 rooms, sectioned into a waiting area, one labour room, 2 wards and a nurses’ quarter.
Like makeup on a corpse, the facility bears a fresh coat of paint. Yet the building’s glowing facade is betrayed by a leaky roof and damp ceilings that hardly keep the workers and patients from the harsh rays of the sun.

“We need help here,” Joseph lamented. “We are doing our best to serve the community, sometimes even touching our salary to ensure that the community gets healthcare, but the facility needs an upgrade. The doors to the labour room are bad, we don’t have electricity and we don’t have a cold fridge to store vaccines,” which hampers the facility’s capacity to carry out routine immunization.
Joseph added that another major challenge of the facility was the toilet. “This is what we use,” he said, pointing to a small pit latrine some 10 feet away from the labour room. “There are times when a patient who has already been admitted goes home just because they don’t want to use this toilet,” he said.
The situation was even deplorable at the Adumbe Primary Health Center in Mbakwen ward, located in the same Gboko Local Government Area in Benue State. With only a motorcycle track leading to it, it takes at least two hours on that path before one sees a vehicle headed for Gboko main town, at least another hour from there.
A community member, Terna Ortse, said the community depends on the Primary health centre for now, even though the chances of survival for anyone who needs emergency care are slim, as the road out of the community is bad.
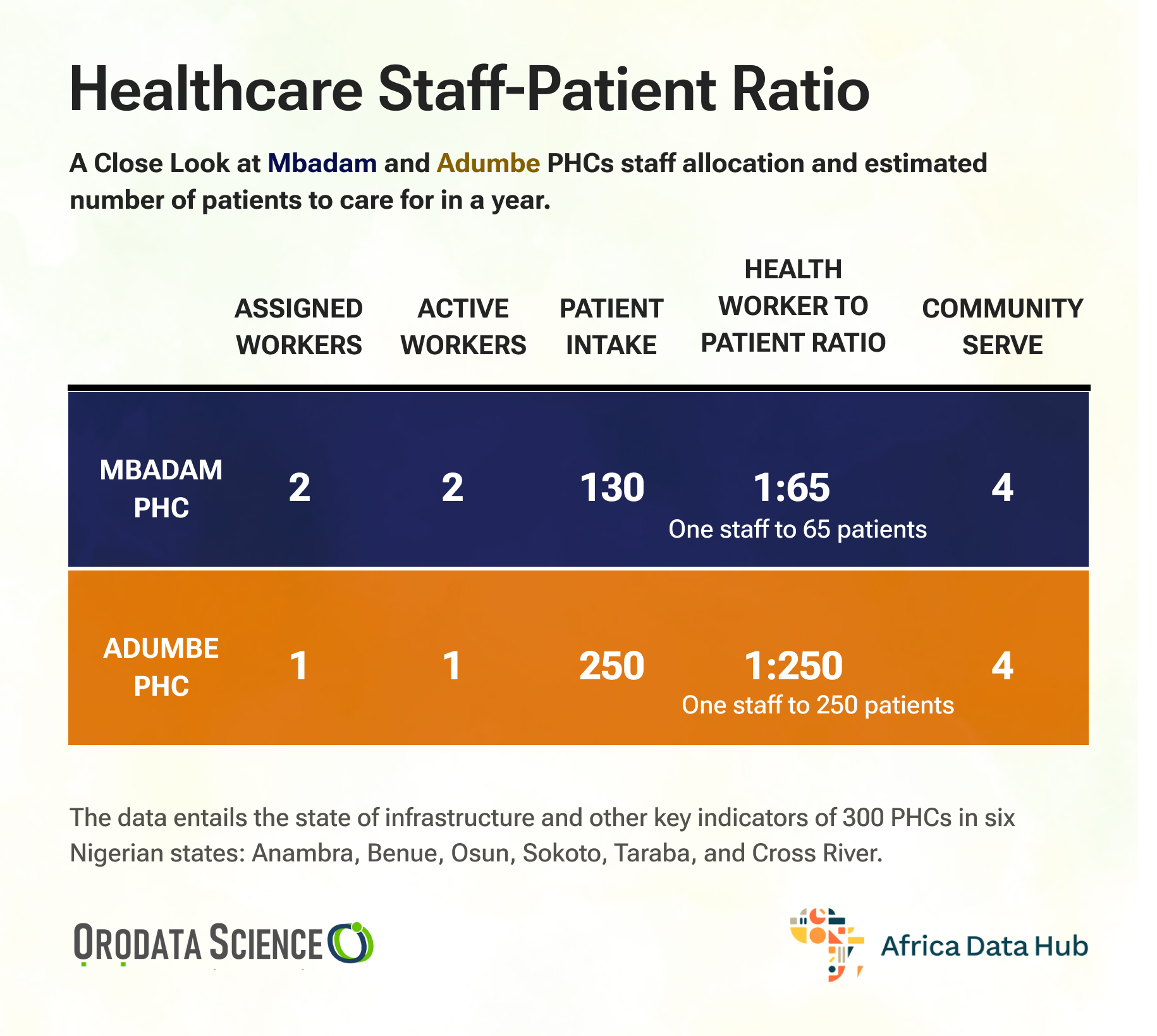
The officer in charge of the facility, identified as Grace Oji, stated that she lives in the facility and is on shift for 24 hours, as she is the only one posted there. “Sometimes I get my daughter to assist me because it becomes overwhelming,” she said. Oji assumes the roles of security, cleaner, lab technician, nurse, midwife and counsellor since “the facility lacks a lot of things.”
The facility has no flush toilet, no fence, and is just three rooms-one which serves the dual purpose of the OIC’s office and labour room, the other which serves a labour room, and the third room where she sleeps.

This is the case in most of the health centres visited by this reporter across various wards in the Gboko Local Government Area. In all the facilities, there were no medical doctors, only one facility had a nurse, and most facilities lacked basic healthcare equipment resulting in poor healthcare outcomes for the state.
Result of abandonment
The Primary Health Care system is to be “the most inclusive, equitable, cost-effective and efficient approach to enhancing people’s physical and mental health, as well as social well-being,” according to Check Msughaondo Isho, a public health practitioner.
Isho, the executive director of Shape African Health, a non-profit that aims to improve the quality of health in society through evidence-based research, and sustainable intervention, the “primary health care system is the backbone towards implementing Universal Health Coverage (UHC)as it serves as the initial point of contact for individuals and families seeking medical assistance,” but in Benue Nigeria’s food basket, that is barely the case.
Years of neglect and government underfunding have led to a loss of trust. As of 2019, Primary healthcare centres accounted for 85.2% of the 39,983 hospitals and clinics in Nigeria, according to the FMoH’s health facility registry (HFR) database. At least 70% of Nigerians rely on it, although only 20% of the PHCs are wholly functional.
For years, Benue State has grappled with a significant gap in healthcare funding. According to research, the state’s budget allocation to health between 2011 and 2025 was woefully low, consistently below the recommended 15% set by the Abuja Declaration and WHO’s 5%. In 2024, the state raised its health budget to 15%, yet observers are still sceptical of fund releases or the impact that would have on health outcomes.
Isho reiterated that this lack of finance affects the ability of the Primary healthcare system to get necessary equipment and to keep the best hands resulting in their inability to offer the best of services. Check held that “Due to the poor infrastructure and lack of machines and equipment in the PHC trained and experienced health workers refuse to go down to these communities and practices-” of the eight centres visited by this reporter across eight wards in Gboko, none had a medical doctor and only one- Adumbe Primary Health care centre- had a trained nurse on sight.
Worse, none of the facilities visited possessed half of the requirements for a Primary Health Care Centre contained in the Minimum standards for PHC’s document published by the National Primary Health Care Development Agency.
A state in Need of quick action
Isho held that a collapse of the primary healthcare systems holds dire consequences for any state, especially one like Benue. About 5.7% of adults aged 15–49 in Benue have HIV, a number that is higher than the national average of 2.1%. This means that out of every 100 people in Benue, around 6 have HIV and for most of these people, Primary health care is their first port of call, and an ill-equipped facility puts them and others around at a disadvantage against the virus.
Also, this shortage of equipment and manpower shows in the state immunization coverage. Despite immunization being both free and mandatory in Nigeria, Benue State falls short, with only 63% of children fully vaccinated according to the 2021 MICS/NICS survey. This leaves a significant portion of the population vulnerable to preventable diseases.
Isho held that more interventions in primary health care (PHC) across low and middle-income countries could increase average life expectancy by 3.7 and save 60 million lives by 2030.
When the reporter visited the Benue State Primary Health Care Board office in Makurdi, a staff member questioned the reporter about their purpose. The reporter explained that they needed to speak with the executive secretary about the state of healthcare centres. However, they were informed that they would need to come back when a new head of the board is appointed.
To turn the tide, Isho argues, “Communities should be involved in the establishment of the facilities and let them be considered in the staffing of the facilities.”
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science
Nigeria’s primary healthcare system faces significant challenges, exemplified by Benue State. Rural communities rely on poorly staffed and inadequately equipped public healthcare facilities like the Mbadam Primary Health Care Centre, which is scarcely visited due to its lack of resources. The facility includes a small bungalow with limited rooms and a deteriorating infrastructure.
Joseph, a staff member, highlighted the center's dire needs, such as a lack of electricity, inadequate storage for vaccines, broken labour room doors, and insufficient sanitation facilities. The Adumbe Primary Health Center is similarly hindered by a lack of staff and basic amenities, affecting the community's access to emergency care.
Despite efforts, healthcare centers in the Gboko Local Government Area suffer from a lack of medical doctors, insufficient equipment, and generally poor healthcare outcomes due to underfunding and neglect. The reliance on the primary healthcare system, which is supposed to be cost-effective and inclusive, is undermined by budgetary constraints and infrastructural deficits. Inadequate funding, despite recent budget increases, continues to hinder service delivery.
Research indicates that only about 20% of Nigeria's primary healthcare centers are fully functional, although 70% of the population relies on them. The gap in healthcare funding over the years has led to poor health outcomes. Adding to the crisis, Benue State's immunization coverage is subpar, leaving many vulnerable to preventable diseases.
The state's HIV prevalence is much higher than the national average, making the role of primary healthcare even more critical. Effective interventions and community involvement in the healthcare system are essential to mitigate the looming public health crisis.
Ultimately, to address these issues, more inclusive and adequate funding, better infrastructure, and community involvement in healthcare staffing and management are imperative. This story highlights the critical need for urgent action to revitalize Benue State's healthcare system.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science.






