Non-communicable diseases such as diabetes and hypertension are increasing across Nigeria, although most cases are detected in their late stages.
The International Diabetes Federation reports that about 3 million Nigerian adults live with diabetes. Yet around 80% do not know they have diabetes.
Routine medical checks are uncommon among low-income citizens, who have to foot their medical bills.
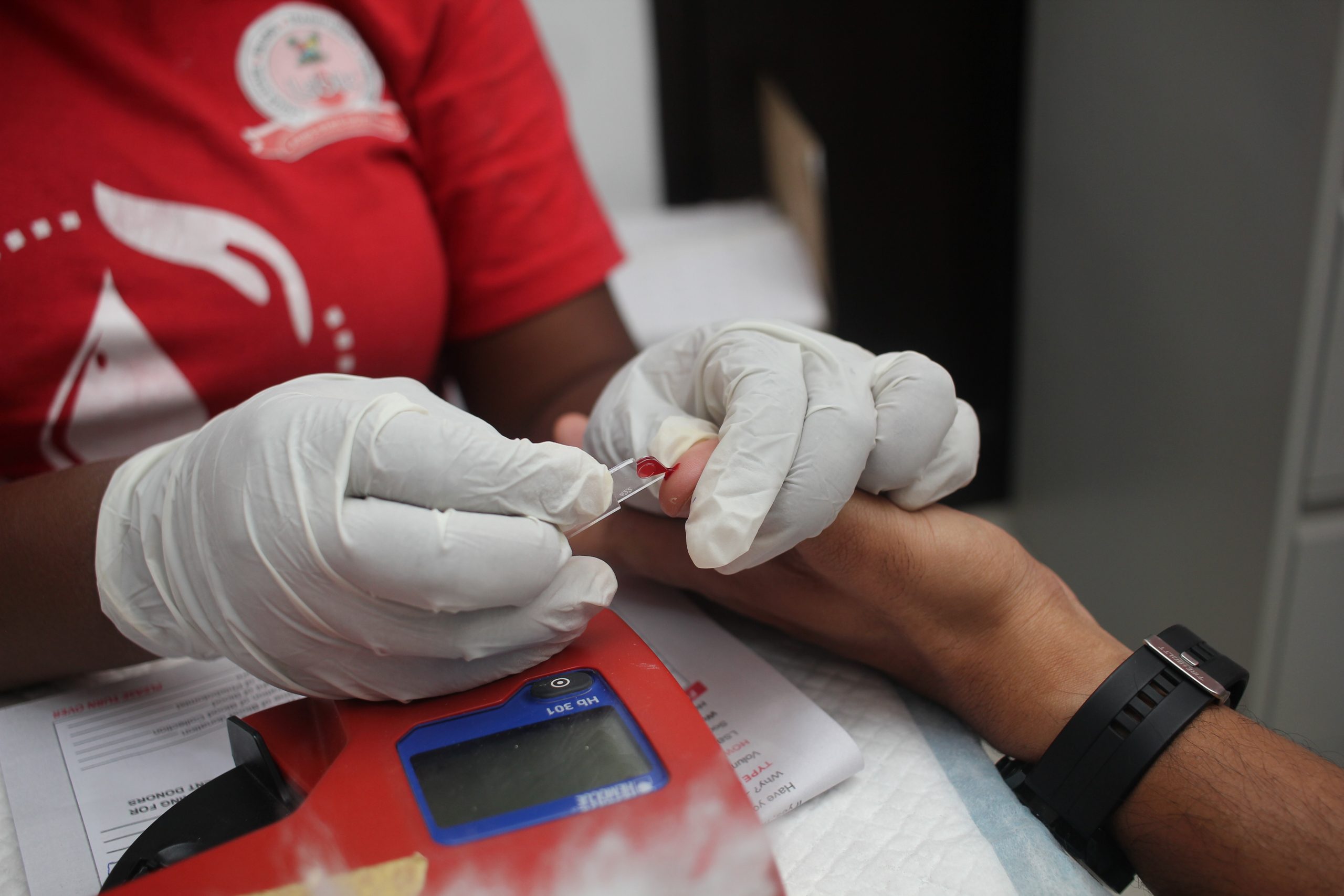
This national challenge framed a recent screening exercise in Nyanya, a dense suburb in Abuja, where more than 400 residents tested for blood sugar, blood pressure and general cardiovascular risk.
The initiative was hosted by the West Africa Postgraduate College of Pharmacists, FCT Zone, and MegaLife Sciences.
Only a small fraction of public-health facilities provide diabetes care, and blood sugar testing remains uncommon, with surveys showing that only 28% of Nigerians have ever had their blood sugar checked.
This gap in detection is not unique to Nigeria. Its challenges mirror Africa’s diabetes crisis. The International Diabetes Federation estimates that more than 24 million adults in Africa are living with diabetes, and roughly 73% of people with diabetes do not know they have it.
These challenges are driving a nationwide push for community screenings and early detection.
For instance, the Federal Capital Territory Administration launched a mass screening programme, testing 250,000 residents across Abuja for diabetes and hypertension.
The Abuja Municipal Area Council has also carried out periodic screenings specifically targeting traders, transport workers, and other previously unserved groups.
Outside Abuja, other states, such as Ogun, also embarked on a more regional approach, taking part in Project 10 Million, which is a nationwide programme to provide free screening and primary counselling to millions.
These efforts reflect growing recognition that early detection is one of the most cost-effective ways to confront Nigeria’s rising non-communicable disease burden.
Nevertheless, screenings alone are not enough. A considerable number of those identified do not have access to finances and available medical care to provide long-term support.
Without reliable follow-up, treatment adherence remains low, and the gains made through early testing risk being lost.
A continental shift in public health
However, there is much to be learnt about the Nyanya programme and affordable care approaches because it demonstrates that community-based interventions can identify those at risk and prevent avoidable complications.
As similar initiatives expand across Nigeria, the hope is that early detection will become routine rather than exceptional—transforming silent diseases into manageable conditions and helping millions live longer, healthier lives.
What is unfolding in Nyanya reflects a much broader African health challenge and, increasingly, a shared continental shift toward early detection as a cornerstone of public health.
Summary not available at this time.