Across Africa, obesity and related non-communicable diseases such as diabetes are rising rapidly, prompting growing interest in breakthrough weight-loss medications like semaglutide-based drugs.
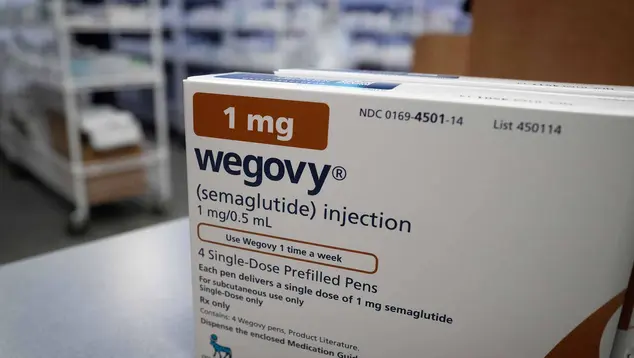
These medicines—including Wegovy, Ozempic and tirzepatide formulations—have shown significant efficacy in clinical trials and are increasingly recommended as part of obesity treatment strategies.
But in much of Africa, the cost of these treatments remains prohibitive, limiting access to wealthier urban patients while leaving the majority behind.
Tackling this affordability gap will require coordinated action across policy, manufacturing and healthcare financing systems.
At present, prices for semaglutide products in African settings are often steep. In South Africa, for example, semaglutide injections can cost between roughly R2,700 and R6,200 per month — amounts far beyond most households’ means and likely confined to private markets.
This mirrors global patterns: when sold in high-income markets without insurance subsidies, weight-loss drugs can exceed $1,000 a month.
To move from niche access to broad affordability in Africa, multiple levers must be pulled simultaneously.
Perhaps one effective long-term strategy is to increase local production of generic versions of weight-loss drugs. Generic medicines can be priced 60–90% lower than branded counterparts because they eliminate patent markups and branding costs.
Currently, patents can restrict generic production, keeping prices high. But TRIPS flexibilities under the World Trade Organisation allow countries to issue compulsory licences or otherwise adjust intellectual property rules to prioritise public health.
By using these flexibilities, African governments could manufacture or import generic weight-loss drugs once patents allow, reducing dependence on costly imports.
Investments in local pharmaceutical capacity—from manufacturing plants to quality assurance systems—would not only lower costs but also strengthen health system resilience and reduce vulnerability to global supply disruptions.
Pooling demand across multiple African countries could strengthen bargaining power when negotiating prices with manufacturers. Regional pooled procurement mechanisms can secure bulk discounts and ensure more transparent pricing, much like approaches used for vaccines and HIV drugs.
A coordinated African strategy could include joint tenders, shared regulatory processes and unified quality standards, reducing fragmentation and improving economies of scale.
The WHO Africa Region’s 10-year roadmap for affordable medicines underscores this direction, calling for coordinated supply chains and market-shaping strategies across borders.
High import duties, value-added tax (VAT) and regulatory bottlenecks often inflate drug prices at the point of sale. Eliminating or reducing these charges for essential medicines—including weight-loss drugs—can make them meaningfully cheaper for consumers.
Governments can also streamline registration and approval processes to speed market entry for quality-assured generics.
Even with lower drug prices, many Africans lack insurance coverage that would reimburse long-term medication costs.
Expanding universal health coverage and including weight-loss drugs in public benefit packages could spread costs across populations and buffer individuals from catastrophic spending. Subsidies or targeted programmes for high-risk patients could also improve access in low-income communities.
While reducing prices is essential, widening access also demands robust regulatory frameworks and clinical guidance.
Unregulated markets can drive counterfeit or substandard products, undermining patient safety and trust in health systems—a concern already documented in Africa’s broader pharmaceutical landscape.
African regulatory authorities must ensure that cheaper generics meet quality standards and that healthcare workers are trained to prescribe, monitor and educate patients on appropriate use.
Emerging research into oral weight-loss medications—which may be easier to distribute and could cost less than injectable versions—holds promise for broader access in low-resource settings.
Supporting clinical trials and regulatory approval of such alternatives in African markets could widen treatment options and further drive down costs.
Making weight-loss drugs affordable in Africa is both a technical and political challenge. It demands strategic use of intellectual property law, investments in local production, smarter regional cooperation, progressive health financing and strong regulation.
Done right, these reforms could transform obesity care on the continent—shifting these breakthrough therapies from luxury products to accessible tools in the fight against a growing public health crisis.
Summary not available at this time.