Even though it is preventable, cervical cancer is one of the most devastating causes of death among women in low-income countries. In many African countries, it is the second most common cancer in women aged 15 to 44.
The disease originates from the human papillomavirus (HPV), which can be squashed through vaccination.
Yet for millions of girls across Africa, Asia, and Latin America, the HPV vaccine was once inaccessible as a result of the cost, low supply or unavailability in the communities where it was needed most.
In 2022 alone, over 350,000 women globally died from cervical cancer. And a staggering majority of those deaths were reported in low-income countries with limited screening centres and treatment options.
An alliance to deepen HPV vaccination
This was the crisis that pushed Gavi, the Vaccine Alliance, along with health ministries and global immunisation partners, into an ambitious three-year effort to reverse decades of inequity in HPV vaccination.
Beginning in 2021, the campaign set out to close the massive vaccination rates between high-income countries and developing nations. It was an undertaking built on three pillars: making the vaccine affordable, supporting national rollout strategies and bringing vaccination directly to schools and rural communities.
Through large-scale procurement and negotiations with manufacturers, Gavi succeeded in driving the cost of the HPV vaccine down to between $2.90 and $5.18 per dose in supported countries, relatively lower than the $100 cost in wealthier nations.
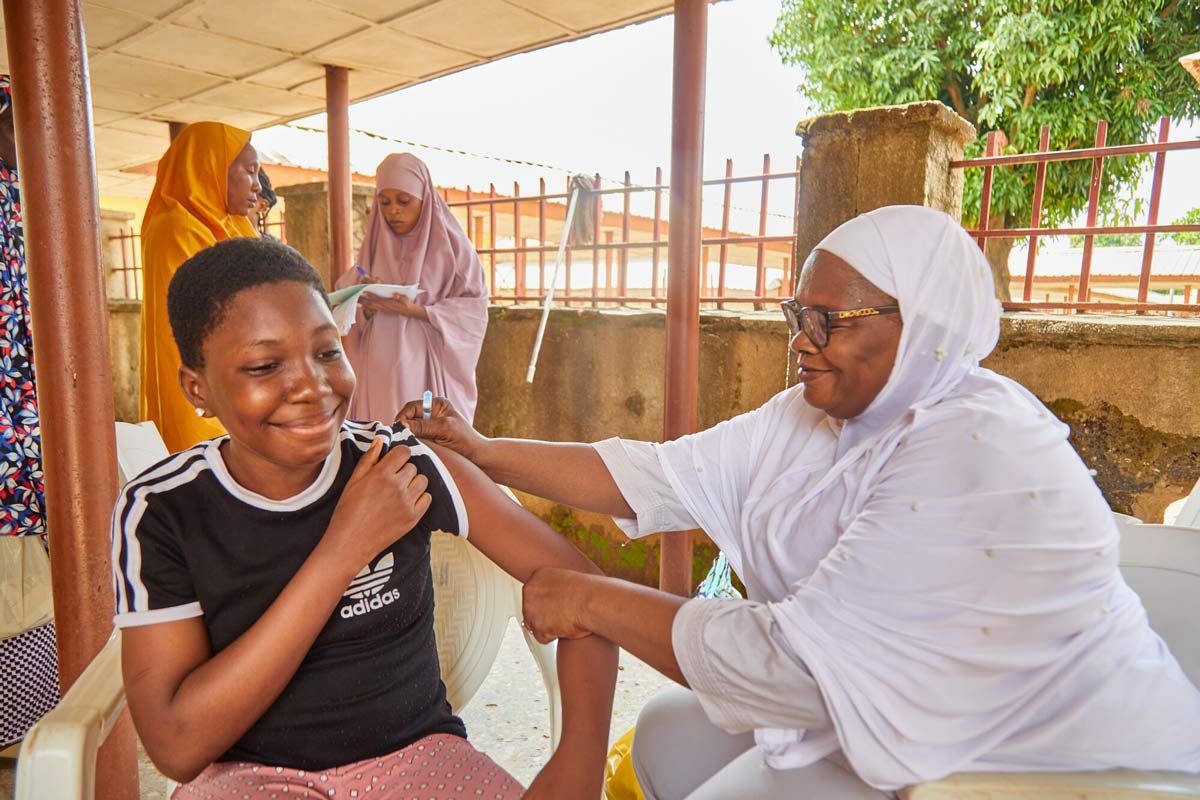
At the same time, countries received financial and logistical support for cold-chain equipment, training of health workers, and community mobilisation campaigns. School-based vaccination drives were launched, and mobile health teams expanded access to remote areas.
The results of this coordinated approach have been transformative. Three years since the campaign began, Gavi reports that 86 million girls across lower-income countries have been protected against HPV, preventing an estimated 1.4 million future cervical cancer deaths.
The impact in Africa is especially commendable. Vaccine coverage rose from just 4% in 2014 to 44% by the end of 2024, surpassing Europe’s 38% coverage.
Countries such as Rwanda, Ethiopia, Malawi, Ghana, Senegal and Kenya have implemented nationwide school-based programmes, targeting girls who, until recently, had never been within arm’s reach of preventive healthcare.
The announcement of these gains, made to mark World Cervical Cancer Elimination Day, highlights one of the most important shifts in global public health in recent years. The momentum was further strengthened, in 2022, by a pivotal decision from the World Health Organisation, which approved a single-dose HPV vaccine schedule.
This policy change made vaccination campaigns more efficient, allowing countries to protect twice as many girls using the same supply. The single-dose HPV vaccine refers to a vaccination schedule where only one dose of the human papillomavirus (HPV) vaccine is administered, rather than the traditional two or three doses.
For communities in difficult-to-reach areas, the single-dose model has reduced missed opportunities and eased the strain on health workers and families alike.
A medley of hurdles threatens this remarkable progress. For example, stigma and cultural barriers persist in certain regions, making community awareness efforts just as crucial as the vaccines themselves.
More investment should be poured into conflict zones, refugee settlements, and rural areas to ensure that no girl is left out.
More importantly, millions of girls now have a fair chance at a future free from cervical cancer. The story of this campaign is a reminder of what can be achieved when vaccines are affordable, when global partnerships are sustained and when communities are placed at the centre of public-health strategy.
Summary not available at this time.