What typically comes to mind when you think of a Primary Health Clinic? Perhaps a welcoming space equipped with cozy chairs and beds, offering comfort to those seeking good health. Unfortunately, this is far from the reality for the people of Affoh in Mbawar Ward, situated in the Gboko Local Government Area of Benue State in North Central Nigeria.
Affoh Community, Mbawar ward in Gboko Local Government Area of Benue State in North Central Nigeria, pregnant women and their children are either forced to travel at least an hour on a motorcycle to access quality health care in Gboko main town or endure the lack of equipment and manpower that plagues this facility deep inside this small community.
John Terver is one such residence. The 27-year-old, first-time dad described the community health centre as no better than a “chemist shop”, and while he appreciated the effort of the staff at the facility when his wife was pregnant, he was forced to take his heavily pregnant wife to the General Hospital in Gboko when she was due.
“It wasn’t as if I didn’t trust the healthcare workers there. I have joined my wife for ante-natal a few times and what I saw there, regarding how the facility looked. I just imagined what would happen if there was a complication and I didn’t want to risk the life of my wife,” he said through a Tiv interpreter.
Terver held that like him, most of his friends with pregnant spouses are concerned about the facility’s state. “It is a different thing if you are talking about a headache or even malaria, but for pregnancy, everyone is concerned as the health centre cannot even admit a patient, as it has no bed,” he stated
“It cost me more to move her to Gboko. She had done her antenatal here, and the staff were very kind and caring, but I knew it was not a gamble I should take. Go there and see for yourself. I am not saying people who allow their wives to give birth there are stupid, but It was not a risk I wanted to take, so I emptied my savings and took her to town,” he said.
It is not only Terver who has the same fear. Joyce Adula said she gave birth to her first son in the facility, but it wasn’t something she wanted to do ever again, saying it was akin to giving birth at home.
“My labour came early, and when my husband rushed me there, nobody was around, and it was call after call before the officer in charge came around. Everywhere was dark and I had to give birth with people staff using their torch light. I am glad there were no complications, but I was always afraid, of things going wrong.” She said.

A facility only in the name
Terver described the Affoh Health Clinic as a clinic only in name, adding that “if you take away the workers from that place it is not even fit to rear pigs in, let alone keep humans who are looking to get healthy,” and he might not be far from the truth.
First, the health care centre is hard to locate, as it is sandwiched between different compounds, close to the Affoh market. There is no signpost, no motorable road, unlike the Catholic Church which is a few distance from it.
When one passes through the other houses in front of the facility and comes face to face with what is supposedly a health facility, you are first confronted with denial and then shock- What is the Affoh Health Centre is two buildings- the first a two-room mud bungalow.
This bungalow has no ceiling, and the roof is rusty and begging for change. Of the two rooms, one is the ward, there, two hospital beds stand in the middle of the room like props, and only one of the beds has a mattress, with a dusty mosquito net hanging over it. The other room, which served as the labour room no better than the delivery bed made sense there, and it still looked out of place with nothing else in the room.
The other building, an uncompleted 5-room bungalow, has one room in use. One where the Officer in charge uses as both his office and the storage room for drugs. This second building has no ceiling, and the outer walls have not been plastered or painted. The floors are not tiles, and the rooms, other than the office of the OIC, have no windows.
This facility does not meet the minimum standard for Primary Health Care in Nigeria as set by the National Primary Health Care Development Agency or NPHCDA.
According to Chapter Three of the minimum standard for Primary Health Care in Nigeria, the health post (which is the lowest in the primary health care cadre) should span a minimum land area of 1,200 square meters, have two rooms with cross ventilation, functional doors, and netted windows, along with separate male and female toilet facilities supplied with water. The facility should also have a motorised borehole for clean water, a power supply, a sanitary waste collection point, a waste disposal site, clear signage visible from entry and exit points, fencing with gate and generator houses, and staff accommodation consisting of 2 units of 1-bedroom self-contained apartments.
Bad facility, worse health outcome
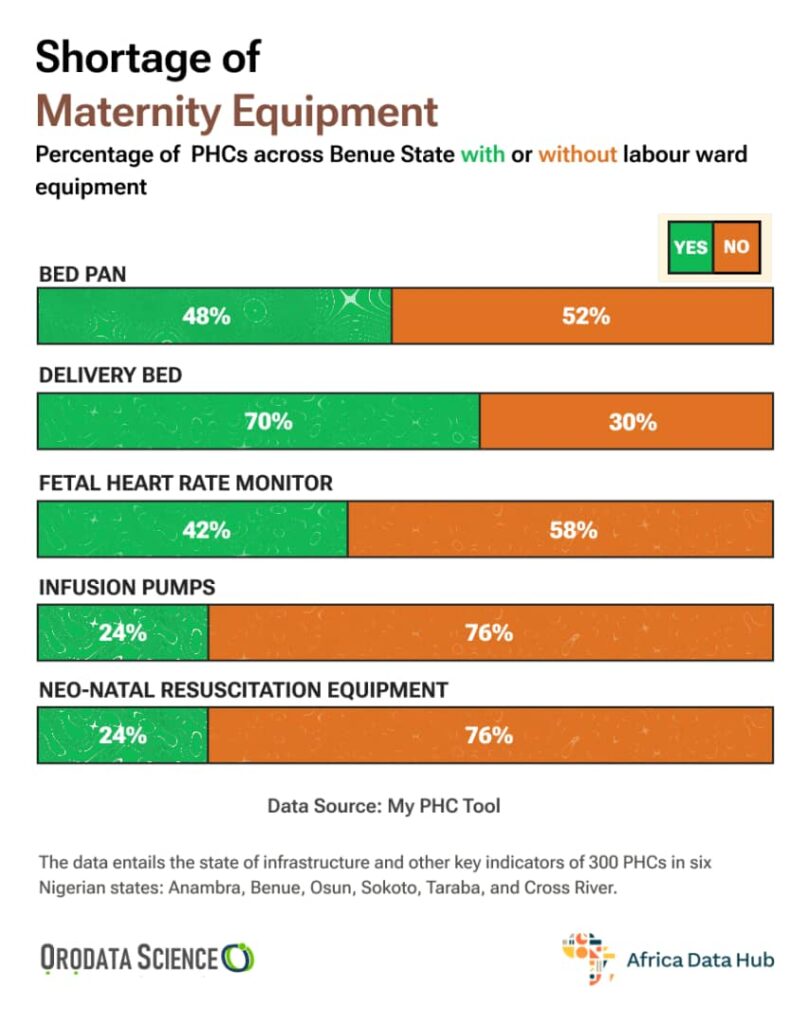
Terver and Adula’s concerns stem from reality rather than fiction, particularly in Benue State. The absence of adequate healthcare infrastructure in areas like Affoh directly contributes to dire health consequences for pregnant women and children within those communities.
Research conducted in Gboko revealed that as high as 14.9% of pregnant women in the area faced risks of mortality or morbidity. In addition, while Nigeria, Africa’s largest democracy has a maternal mortality ratio of 512 per 100,000 live births, as of 2018, Benue State, one of Nigeria’s 36 states, reported a significantly higher maternal mortality ratio of 1,189 per 100,000 live births, more than double the national average.

The number gets worse, according to the 2021 Nigeria Multiple Indicator Cluster Survey or MICS report, in Benue, one out of every 56 newborns die within the first 28 days, while a further 42 out of every 1,000 live births fail to reach their fifth birthday.
Need for more investment in Primary Healthcare
In 2023, Budgit, a civic tech platform focused on budget transparency, revealed only 9.67% of Benue state’s total spending for the period was for healthcare (inclusive of capital and recurrent expenditure). Shockingly, the state’s health spending per capita amounted to just N1508.52 in a state where “just 2.5% of women in Benue are covered by health insurance, which is below the average coverage for the northcentral region,” the document states.
On his part, Isho Check, a public health practitioner with Shape Africa Health held that PHCs are the foundation for universal health coverage, and a more inclusive approach of better financing and community involvement will help stop the tide of rot that has bedevilled the sector.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science





