While collecting firewood in a remote forest in Lubombo, eastern Eswatini, a deadly black mamba snake bit 29-year-old Cindy on her lower thigh.
As she screamed in pain back in her village, someone from the neighbouring homestead quickly brought a concoction for her to drink. Desperate, she drank the bitter contents before a friend rushed her to the hospital.
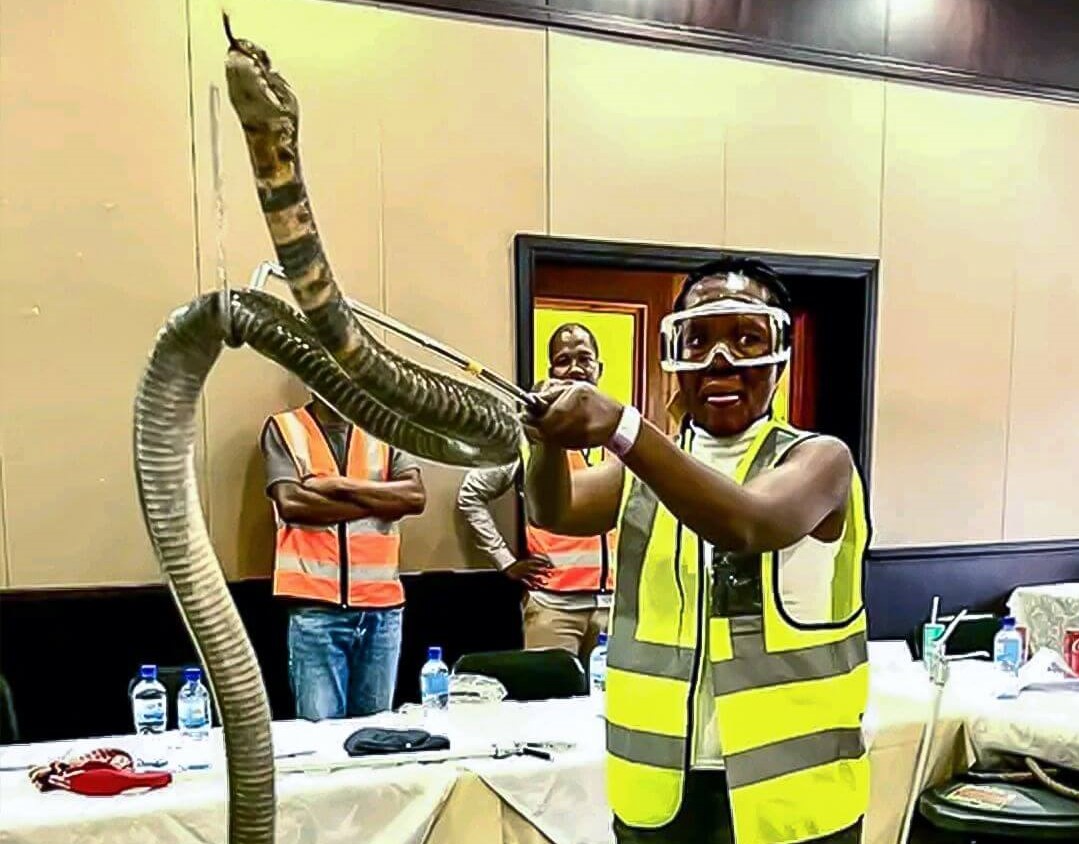
Thea Litschka, Eswatini’s only woman snake handler and founder of the Eswatini Antivenom Foundation, was on duty at the hospital that day and recalled that Cindy (surname withheld) was brought in with classic black mamba symptoms: sweating, restlessness, nausea, and respiratory distress.
However, there was also blood in her vomit.
The team attending to Cindy thought it had made a mistake with the diagnosis because, Litschka explained, black mamba snakebite victims do not bleed profusely internally.
“Her abdomen was swelling rapidly – something was very wrong,” Litschka said.
A referral was quickly arranged to The Luke Commission (TLC), which still had antivenom and life support critical for advanced black mamba bites.
“Blood units were immediately given. She was also given a large dose of antivenom, but her condition continued deteriorating,” Litschka recalled.
Shortly after that, Cindy’s heart stopped, and she was declared dead a little later. But she did not die from the snakebite.
“We finally discovered that the concoction she drank was so corrosive that it had destroyed her stomach and intestines, which was the cause of the bleeding. She died from the concoction, a supposed traditional snakebite cure.”
Cindy’s case is one of the numerous daily cases that Litschka has handled. Her work in snake conservation and education dates back to 2005.
Many setbacks
However, Litschka’s work has been jeopardised by an unexpected development. The facility that produces antivenom for many African countries – South African Vaccine Producers – was hit by nationwide power outages that crippled production. The unit is now desperately trying to recover its output, but deliveries outside the country have been badly affected.
“Antivenom is an essential medicine – without it, the victim will die or lose a limb. Not having antivenom in Eswatini is beyond unacceptable,” Litschka said.
“Unfortunately, the supplier from South Africa has let the entire southern African continent down. We can’t buy it, even if we want to, and they can’t supply it. I am still waiting for the stock we paid for in November 2021.”
Litschka explained that the countrywide shortage of antivenom means the Eswatini Antivenom Foundation (EAF) volunteers are constantly on call, working with the clinicians from the hospitals and clinics to assess bites and, if necessary, transfer patients to TLC, the only facility that still has vials of antivenom left.
“Despite receiving and treating 110 patients so far, they have never turned us away, and because every bite is carefully assessed and consulted, they have never run out of antivenom. YET!”
Moreover, antivenom is currently very expensive and unaffordable for most people in Eswatini. The cost to treat one Mozambique spitting cobra victim is $1620, and a black mamba bite is $1080 – much more expensive than the average Swazi can afford.
So Litschka and her EAF team, concerned about supplies as far back as 2016, pushed through and found funding to develop a product and put it through pre-clinical testing.
“Sadly, it is taking quite long to get it registered and imported into Eswatini, but we are hopeful it will be in all the health centres and hospitals for the next snakebite season. The cost is also one-quarter of what we are paying now, which will assist with the financial burden for the Foundation and the country,” she added.
In addition, Litschka and the EAF are currently involved in development research for antivenom that will be free to snakebite victims. This research entails studying snake venom to see if it changes in captivity.
“Companies who extract venom for the production of antivenom are not controlled. We suspect that if you keep a snake in captivity for many years and only feed it dead food, the venom composition may change,” she stated.
The study is being conducted on 180 snakes – some are fed dead food only, others only live mice and the third control group, a variety of live food as they would find in natural settings.
Several research projects have since been completed; they are busy with a few more.
Snakebite data from all the major health centres and hospitals in Eswatini was also collected.
A special data book captures data regarding the victim (age, occupation, region), what the victim did when they got bitten, the venom (syndrome) effects, if antivenom was used and the outcome.
“This helps us determine where we need antivenom. We have 15 antivenom banks throughout the country and where education is most needed,” she said. “Then we put the data of snakes rescued in the mix and habitat. We have developed a “Risk Map” together with the University of Eswatini that will help us plan better,” she added.
They have also conducted further studies to look into the effects of Mozambique spitting cobra venom and the effectiveness of the antivenom.
Snakebite assistants were stationed in all the hospitals, who called when a victim arrived and sent pictures.
“I would then tell them if the victims should be included in the study. We monitored the wounds, how big, blisters, blebs, etc. We have also studied the effectiveness of our new antivenom,” she said.
Litschka is confident that these efforts will soon bear fruit and casualties from snake bites will remain a thing of the past in Eswatini.
Bird story agency
While gathering firewood in Lubombo, Eswatini, Cindy was bitten by a black mamba snake and drank a corrosive traditional concoction, leading to severe internal bleeding and her eventual death, not from the snakebite but from the concoction.
Thea Litschka, Eswatini's only female snake handler and founder of the Eswatini Antivenom Foundation (EAF), was involved in Cindy's case. Litschka's efforts in snake conservation and education began in 2005 and face significant challenges due to a shortage of antivenom caused by power outages affecting production in South Africa.
Due to the antivenom shortage, Eswatini volunteers and clinicians must carefully assess snakebite cases and transfer severe ones to the only facility with remaining antivenom stock. High costs and limited availability of antivenom make treatment inaccessible for many. Litschka and her team have been working on developing a more affordable antivenom product since 2016, which is currently undergoing pre-clinical testing.
Litschka is also researching snake venom composition changes in captivity, collecting extensive snakebite data, and creating a "Risk Map" for better planning. These efforts aim to make antivenom more accessible and affordable in Eswatini, ultimately reducing snakebite casualties in the future.